More and more healthcare providers implement clinical decision support systems (CDSS), and these solutions are expected to grow in popularity in the near future. A study shows that the global CDSS market is forecast to expand from $1.2 billion in 2020 to $1.8 billion by 2025.
Why are CDS systems getting traction? It could certainly be the effect of government initiatives and the COVID-19 pandemic. But perhaps the primary reason is that they create real, tangible value for providers and patients.
This article focuses on the benefits and challenges of adopting clinical decision support tools in healthcare workflow. We’ll help you weigh all the pros and cons and top it off with a list of essential steps needed to implement a clinical decision support system successfully.
If you’re looking to improve the quality of patient care and achieve better cost efficiency at your facility, a CDSS might be just what the doctor ordered. Keep reading for the full prescription.
What is a clinical decision support system?

A CDS system is a software tool designed to provide clinicians with relevant medical information to facilitate decision-making or improve adherence to recommended care. You can integrate it into an EHR (Electronic Health Record) or HMS (Hospital Management Software) system or use it as a separate application or part of a patient portal.
The amounts of knowledge and data healthcare professionals deal with can be overwhelming. The idea behind CDS systems is to offer the much-needed support in finding, processing, and delivering information quickly and at the right moment.
For example, CDSS can compare a patient’s medical history and known allergies to the current symptoms in real-time and present a doctor with a list of potential diagnoses. This software can also display an alert that tells a nurse to administer medication in a different dosage due to a change in the patient’s condition.
However, a CDSS is by no means a fully automated decision-making solution. It only helps doctors narrow down their choices and decide on the course of action or assists nurses in following a treatment plan. But let’s get more specific. What promise do these tools hold, and how can your facility get the most out of implementing a clinical decision support system?
The main benefits of implementing a CDSS

CDS tools can streamline your organization’s workflow in a variety of ways. With proper implementation of a clinical decision support system, here is what you can expect to achieve.
Enhance the diagnostic process
The first and greatest advantage of implementing a CDSS is its round-the-clock availability as a mechanism for diagnosing patients.
CDSS are very efficient at translating symptoms into a diagnosis. An approach known as case-based reasoning (CBR) can be used in healthcare in combo with AI to help doctors make correct conclusions. Once a CDS tool is integrated with a well-designed EHR/EMR system, the software can access patient data and process it to suggest a range of possible diagnoses.
Such data can include pre-existing conditions, allergies, previous hospitalizations, current medications, an account of symptoms, and test results. With appropriate computing power, the right algorithms, and a knowledge base in place, the response will be instantaneous.
Technologies like big data analysis and cloud computing can take your CDSS another step further. Just imagine having an advanced analytics system that can identify undiagnosed conditions and predict treatment outcomes. It may sound like a phrase from a sci-fi novel, but it’s absolutely achievable today—with the right software vendor.
Improve the quality of care
Modern CDS software can analyze data and automatically generate alerts — reminding of a routine visit or a planned medication order or flagging a potentially dangerous condition. This functionality is especially valuable when dealing with chronic diseases. It can also cut hospital readmissions and improve the patient’s quality of life.
For instance, if a patient admitted to your clinic has a record of CVD (cardiovascular disease), critical low-density lipoprotein (LDL) levels can make the CDS module trigger an alert.
Similarly, the system can send a reminder to a nurse to measure blood glucose in line with the protocol. This simple action may prevent hypoglycemic episodes in patients with diabetes.
CDSS can also keep track of the schedule of follow-up visits to the doctor’s office or home care visits.
Prevent medication errors
Since CDSS are capable of generating event-driven alerts, they can help fight problems on yet another front. New data from a patient’s test results or monitor readings can trigger a CDSS to intervene and recommend changing the medication type or dosage.
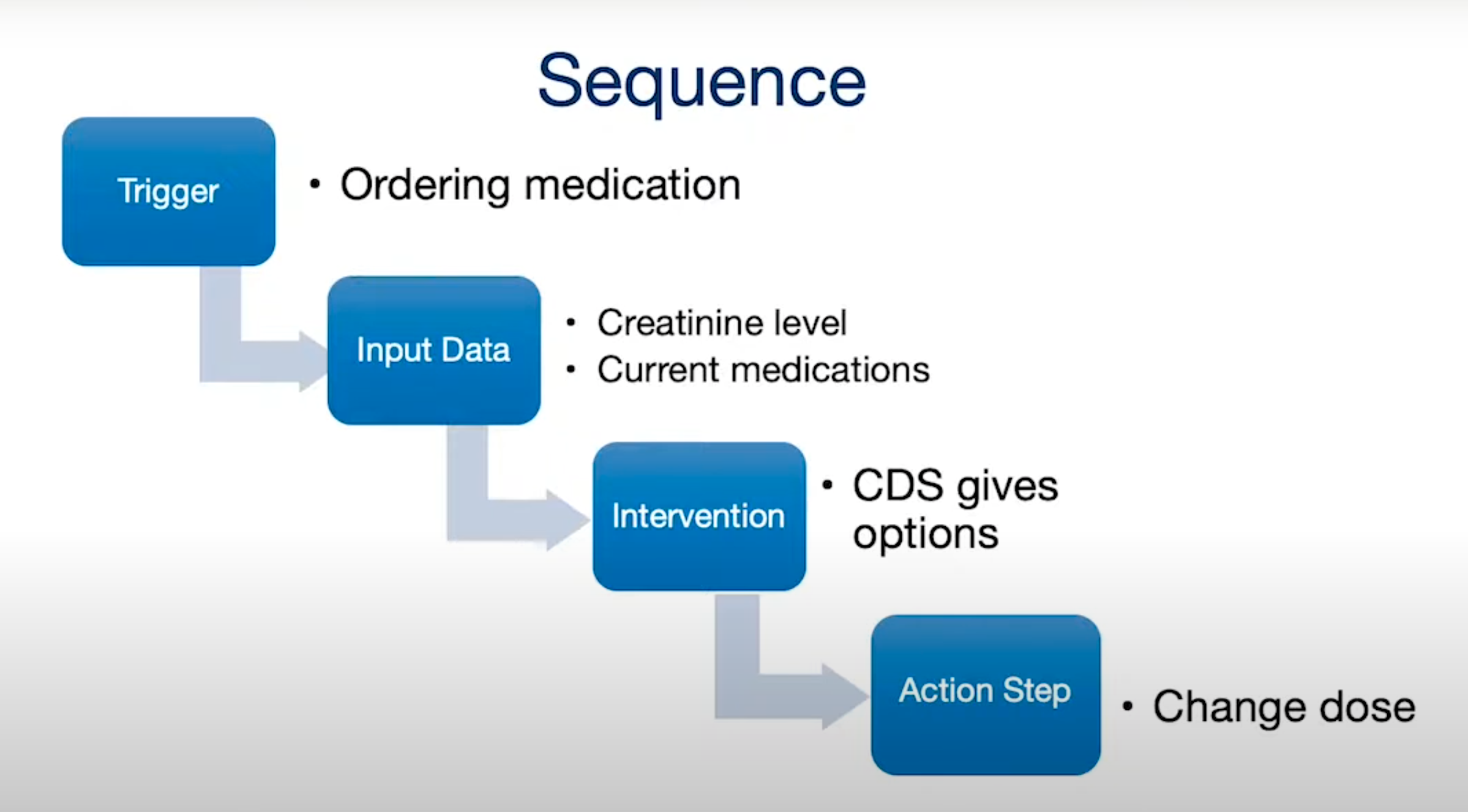
A recent NCBI study states that distraction is the cause of 75% of all medication errors in medical facilities. A CDS module could prevent this by automating the order process and generating informative alerts at the right time.
DDI, or drug-to-drug interactions, is a critical consideration in the process of prescribing medications to patients. Some drugs may cause unfortunate side effects if accidentally administered in combination. Properly set up CDS software could reduce or completely eliminate the chance of this happening.
Streamline administrative functions
Reducing the administrative burden is another significant improvement made possible by CDSS.
Errors in medical coding can delay medication and procedures orders or cause subsequent claim denials. To avoid these pitfalls, you must have your CDSS match the latest code standards and contain document templates.
The same goes for improving document flow and accuracy. A properly set up CDSS system can aid physicians in filling out clinical documentation. The software can also alert if patient data is inconsistent or flag situations that require the clinician’s attention.
When it comes to admitting, transferring, and discharging patients, implementing a clinical decision support tool can help automate routine paperwork.
Planning medication orders is also a lot easier with a system that contains and manages standard order sets for typical medical conditions and scenarios.
Reduce readmission rates and save costs
Better diagnostic practices and more effective treatment, along with scheduled home visits, will improve patient outcomes. Readmission rates will gradually go down. The resulting cost savings will be the cherry on top.
Read also: How to Reduce Hospital Readmission Rates
CDS software can help you reduce human error to a bare minimum while automating and streamlining most decision processes that are crucial for a profitable medical business.
Cutting down on the number of imaging orders is a great example. A CDSS can optimize the types and quantities of medical imaging — saving a lot of costs — by comparing patients’ symptoms with a database of previous cases. You can apply the same principle to other costly tests, so you don’t have to pay for overtime hours spent on pointless jobs.
Is there a secret recipe for integrating clinical decision support tools into your facility’s workflow? Let’s find out.
Adopting a clinical decision support system in 10 steps
It’s safe to assume that your medical organization has an established set of procedures and applications in place. We recommend following these ten industry-proven steps for your new CDSS to fit seamlessly into the ecosystem.
Step 1: Define your objectives
Every business endeavor starts here. What do you plan to achieve with the new CDS software? What pain points does your medical facility have that need to be covered? Set realistic goals, rough timelines, and quantifiable KPIs.
Step 2: Get buy-in from stakeholders
It’s time to get everyone on board with the idea of a new CDS software. Hold a meeting and explain its benefits for the business. Key stakeholders must clearly understand all the factors that shape the cost of implementing a clinical decision support system.
Step 3: Ensure that quality data is available
It’s crucial to review your current data sources — their accuracy and compliance with privacy and interoperability standards. Hopefully, your organization has been keeping up with the data exchange standard trends, and your employees have been entering the patient data correctly.
Step 4: Find a software vendor
This step is unavoidable unless you have an in-house IT team with the necessary skillset and experience. Study reviews, portfolios, and client testimonials when searching for a software partner. Use resources like Clutch.
Step 5: Determine the scope of features
At the planning stage, discuss your objectives with the development team. You don’t need a generic product but a solution custom-tailored to your specific needs.
Step 6: Find the best integration strategy for your workflow
Consult with your software vendor to determine the best way to integrate the future product with your legacy applications, data sources, etc. If necessary, the developers can refactor some code to achieve better compatibility.
Step 7: Receive an MVP and provide feedback
A Minimum Viable Product is your perfect opportunity to get a sneak preview and give valuable feedback to the developers. It can save lots of money and time and prevent massive rework later.
Step 8: Fine-tune according to your needs
Work in tandem with your vendor to adjust the features to your specific requirements. A good CDS solution should fit your workflow like a glove.
Step 9: Get a working product with proper support
Receive a stable version of your new CDSS and take it out for a spin. Make sure your contract with the software vendor includes a clause on support and updates.
Step 10: Complete personnel onboarding and reap the benefits
As we mentioned earlier, a reputable vendor will likely assist you with onboarding. Taking pains to train your staff now will definitely pay off later.
But you also have to be aware of the possible obstacles for the implementation process to go smoothly. Reading the next section will help with that.
The typical challenges of implementing a CDSS

CDS systems have been around for almost 30 years, so many quirks have been ironed out, myths debunked. Still, there might be some bottlenecks in adopting these tools. Luckily, most of them are temporary and/or easy to overcome.
Lack of interoperability
Ironically, what was intended as one of the most notable benefits of CDSS is also among its biggest shortcomings. We’re talking about data silos and poor interoperability, of course.
However, this is not exclusive to clinical decision support systems but rather reflects the current state of affairs in healthcare. Even though most software vendors realize the importance of data exchange standards, many hospital systems are still isolated and fail to communicate effectively. Your best bet here is to create a CDSS that supports all modern standards like HL7 and FHIR while carefully picking compliant data sources.
Privacy concerns
This is another factor that slows down the implementation of advanced clinical decision support systems. As with any software that involves data management, there are risks associated with storing and transferring sensitive patient data. Note that compliance with the Health Insurance Portability and Accountability Act (HIPAA) is mandatory for such software in the US.
The key to overcoming this data breach challenge is to use secure data transfer protocols and adhere to high security standards in general. With an experienced software partner, developing a HIPAA-compliant CDS solution should not be a problem.
Dependence on external data sources
A CDS system’s ability to generate relevant alerts and diagnostic suggestions largely depends on the quality of input data. If the source information is error-ridden or rarely updated, it may lead to dangerous consequences.
Reliable data sources and regular updates can save you from those headaches. Once again, we recommend working closely with your software vendor on this matter.
Disruptions in workflow due to poor implementation
Alert fatigue is one of the common causes of frustration and burnout among physicians working with CDS systems. Multiple alerts of varying relevance and critical importance that constantly pop up on the screen can easily disrupt concentration. After a while, doctors and other medical staff tend to become overwhelmed by the sheer number of alerts generated by CDSS. A recent study suggests that this may even lead to a drop in safety standards.
Balancing high- and low-priority alerts and using machine learning mechanisms could help avoid such disruptions.
Read also: Machine Learning in the Medical Field
Resistance to innovation
Any new tool you introduce to your staff comes with a learning curve. Many doctors and nurses have had a bad experience with CDS systems and might be reluctant to engage with the new software.
But if that software is well-designed and has no usability issues, your employees will appreciate its positive effect quite soon, and their attitude will inevitably change.
Summing up
CDS systems are clearly past their infancy and adolescence and are entering maturity. Big data analysis, AI, cloud computing, and machine learning — these technologies are now casually integrated into CDSS to assist clinicians in their day-to-day work. And, as we all know, technology only gets better with time. So there’s really no sense in waiting for the perfect moment.
Also, it seems that the benefits of implementing clinical decision support systems into the software ecosystem of your hospital outweigh the possible challenges. To ensure the best outcome, it’s important to choose a vendor with relevant experience and a portfolio of successful projects.
Working with Demigos, you get the perfect blend of profound healthtech expertise, versatile development skills, and the most rigorous testing. We never compromise on quality, always bringing our best game. Get in touch with the team, so we can discuss the details of your project.






